Nanoparticles can reveal lung disease
Nanoparticles can be used to discover illness in the lungs. The method of measurement – based on inhaling particles – is easy to use and could serve as a complement to other lung examinations. The method has now been tested on more than 800 people, and the results look promising, according to a new thesis on aerosol technology at the Faculty of Engineering (LTH) at Lund University in Sweden.
Jessika Sellergren – Publicerad den 30 May 2023
Measuring the structures of the lungs is difficult. Not even chest x-rays can reliably capture changes in the alveoli, the lung’s smallest components. The new measurement method, AiDA – Airspace Dimension Assessment – can provide more answers about precisely those smallest tissue structures in the lung.
The method has been used on more than 800 participants. The method has also been compared with established techniques such as chest x-rays, pulmonary function tests and MRI scans with hyperpolarised gas.
Madeleine Petersson Sjögren, one of the researchers who studied and evaluated the technique, has now presented her results in a thesis on aerosol technology. She says:
“Our results show that the method can be used to identify pathological changes in the lung. The method is fast and provides results that, according to our research, match those of more advanced methods of measuring the structure of the lung.”
The number of particles that get stuck reflect the structure of the lung
The method is based on the knowledge that nanoparticles move in a particular way in air, and the fact that the tissue structure differs between healthy and sick lungs.
“By inhaling a low concentration of nanoparticles and measuring the number that get stuck, we can calculate distances inside the lung which is a measure of how large the cavities in the lungs are. That distance can reveal whether there are pathological changes or not,” says Madeleine Petersson Sjögren.
In a healthy lung, the alveoli are small, well-defined and have short distances between the tissue parts. As a result, there is a lot of surface area on which the particles can get stuck, which means that few particles are exhaled. In a diseased lung, the opposite is the case:
“If you have emphysema, the alveoli are broken down and you get larger cavities in the lung. That means there is less surface area on which the particles can get stuck, resulting in more particles being exhaled.”
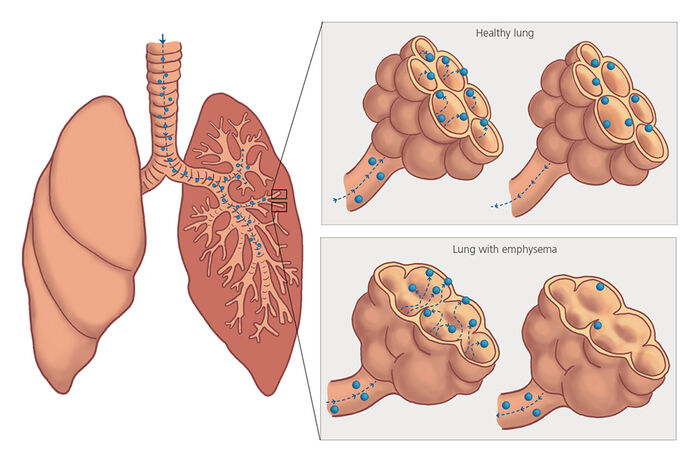
In a healthy lung, the alveoli are small, well-defined and have short distances between the tissue parts. As a result, there is a lot of surface area on which the particles can get stuck. If you have emphysema, the alveoli are broken down and you get larger cavities in the lung. That means there is less surface area on which the particles can get stuck. Illustration: Johanna Rydeman/Pexels
The structure of the lung is changed when we contract lung diseases, but according to Madeleine Petersson Sjögren these changes can be difficult to identify using conventional methods such as x-rays and pulmonary function tests.
“Since today’s methods of lung diagnosis are often insufficiently sensitive to changes in the deepest parts of the lung where diseases such as emphysema take hold, the disease has often progressed by the time it is discovered, making it more difficult to restrict.”
A quick examination – and no radiation
As well as the method being able to reveal serious illness at an early stage, it is also quick to conduct and does not entail any significant discomfort for the patient.
“An examination takes around fifteen minutes and the number of particles the patient inhales is comparable to the concentration present in the air in our day-to-day environment,” says Madeleine Petersson Sjögren, whose research also compared the technique with other methods of measurement such as chest x-ray and MRI scans using hyperpolarised gas.
“The results from the various methods of measurement match – that suggests that AiDA could be a useable method for early diagnosis of pulmonary disease,” says Madeleine Petersson Sjögren.
Other advantages she can see are that the method does not expose the patient to radiation, as with chest x-rays, and that the technique could be made widely available. MRI technology is more advanced, but inaccessible and expensive – it is only present at a few sites around the world.
May be useful for other lung diseases
Globally, the third-largest cause of death is Chronic Obstructive Pulmonary Disease, COPD, with emphysema often part of the illness.
“If emphysema of the lung can be discovered at an early stage, the opportunities for restricting the progress of the disease are greater,” says Madeleine Petersson Sjögren.
She also hopes that other pulmonary diseases can be diagnosed using the method in the future:
“In the future we would like to investigate whether the method can be used to identify other pulmonary diseases, such as fibrosis and asthma, for example.”
Madeleine Petersson Sjögren
Madeleine Petersson Sjögren defended her thesis Structure of the distal lung studied with inhaled nanoparticles.
Madeleine Petersson Sjögren in Lund University research portal
About the AiDA method
The AiDA method of measurement has been in development since 2011, as a collaboration between aerosol technology at LTH and Translational medicine at the Faculty of Medicine at Lund University. The method has so far only been used in research studies and is currently in place at Lund University and Uppsala University. Results from various groups of patients with lung problems have shown that AiDA detects pathological changes in the deep part of the lung that are difficult to measure using conventional methods.
How an AiDA measurement is conducted
The patient breathes clean particle-free air for a few breaths, to empty the lungs of particles. Afterwards, the person takes a deep breath of air containing nanoparticles, holds their breath for five to ten seconds and then breathes out. The quantity of particles in the inhaled air is compared with the exhaled air – the difference being the number of particles that have remained in the lungs. This information makes it possible to calculate the average distance between surfaces in the lung. The distance reveals what the structure of the lung is like and can reveal whether any pathological changes have occurred.
